Understanding Hematochezia: Causes and Implications of Blood in Stools
Hematochezia, the medical term for the presence of fresh blood in stools, can be a distressing and alarming symptom for individuals experiencing it. Blood in stools may range from mild and self-limiting to a sign of a serious underlying condition.
Understanding the causes and implications of hematochezia is crucial for timely diagnosis and appropriate management. In this article, we will explore the common causes of blood in stools, the significance of this symptom, and when to seek medical attention.
Causes of Hematochezia
Hematochezia occurs when there is bleeding in the lower gastrointestinal (GI) tract, which includes the rectum, colon, and anus. Some of the most common causes of blood in stools include:
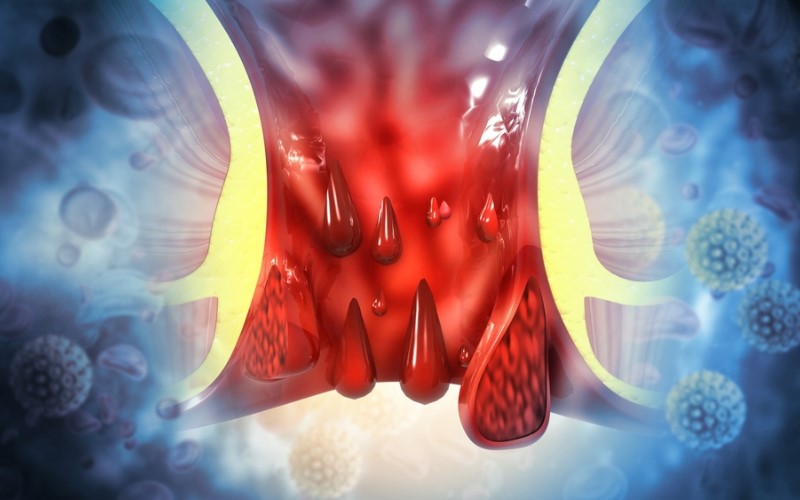
Hemorrhoids
Hemorrhoids are swollen and inflamed veins in the rectum or anus. They are a common cause of hematochezia, especially when blood is seen on the surface of the stool or on toilet paper after wiping.
Anal Fissures
Anal fissures are small tears or cuts in the lining of the anus. They can cause bright red blood to be visible on the surface of the stool.
Diverticular Disease
Diverticula are small pouches that can form in the colon wall. When these pouches become inflamed or infected, they can lead to bleeding in the stools.
Inflammatory Bowel Disease (IBD)
Conditions like ulcerative colitis and Crohn’s disease are types of IBD that cause inflammation in the GI tract, which can result in bleeding.
Colorectal Polyps
Colorectal polyps are growths that can develop on the lining of the colon or rectum. While most polyps are benign, some can be precancerous and cause bleeding.
Colorectal Cancer
Colorectal cancer is a malignant growth that can also cause bleeding in the stools, especially as the tumor grows.
Anal Cancer
Cancer in the anal region can also lead to blood in stools, often accompanied by pain and discomfort.
Gastrointestinal Infections
Certain infections of the GI tract, such as bacterial or parasitic infections, can cause hematochezia.
Intestinal Ischemia
Intestinal ischemia occurs when there is reduced blood flow to the intestines, leading to damage and bleeding.
Peptic Ulcers
Peptic ulcers, which can occur in the stomach or the upper part of the small intestine, can cause blood to appear in stools due to bleeding in the upper GI tract.
Implications of Hematochezia
While hematochezia can sometimes be a result of benign conditions like hemorrhoids or anal fissures, it can also indicate more serious health issues. The implications of blood in stools depend on various factors, including the amount of bleeding, the duration of symptoms, and the individual’s medical history.
Acute Bleeding
If blood in stools is accompanied by significant bleeding, dizziness, weakness, or lightheadedness, it may indicate an acute and potentially life-threatening situation that requires immediate medical attention.
Chronic or Recurrent Bleeding
Chronic or recurrent hematochezia may be a sign of an underlying condition that requires further investigation and management. This can include conditions like IBD, colorectal polyps, or colorectal cancer.
Age and Family History
The age of the individual and their family history of gastrointestinal conditions, including colorectal cancer, can also influence the implications of hematochezia. Individuals over the age of 50 or with a family history of colon cancer may be at higher risk and require earlier evaluation.
When to Seek Medical Attention
Any presence of blood in stools should prompt a visit to a healthcare professional for a thorough evaluation. If the blood is bright red or there are significant amounts of blood in the stools, immediate medical attention is essential.
Additionally, if hematochezia is accompanied by other concerning symptoms such as abdominal pain, changes in bowel habits, unintended weight loss, or weakness, prompt medical evaluation is crucial.
Diagnosis and Evaluation
To determine the cause of hematochezia, healthcare providers may perform a series of diagnostic tests, which can include:
- Physical Examination. A physical examination, including a digital rectal examination, may be conducted to assess for any visible abnormalities in the anus or rectum.
- Colonoscopy. A colonoscopy is a key diagnostic procedure used to visualize the entire colon and rectum to identify the source of bleeding, such as polyps, tumors, or inflammation.
- Flexible Sigmoidoscopy. Similar to a colonoscopy, a flexible sigmoidoscopy focuses on examining the lower part of the colon and rectum.
- Stool Tests. Stool tests may be performed to check for the presence of blood and to rule out infections or parasites.
- Blood Tests. Blood tests can provide information on the overall health of the individual, including potential anemia or signs of inflammation.
- Imaging Studies. In some cases, imaging studies such as CT scans or MRI may be used to evaluate the GI tract and surrounding structures.
Conclusion
Hematochezia, or blood in stools, can be a concerning symptom that requires timely evaluation and diagnosis. While it may be caused by benign conditions like hemorrhoids, it can also indicate more serious gastrointestinal issues, including colorectal cancer.
Seeking medical attention promptly and undergoing appropriate diagnostic tests is crucial to determine the cause of hematochezia and implement an effective treatment plan. Early detection and appropriate management can significantly improve outcomes and ensure the best possible health for individuals experiencing blood in their stools.